Amidst the dynamic landscape of healthcare payer operations, a groundbreaking force, Generative AI, is poised to revolutionize the way payers navigate the intricacies of claims management and patient care. Generative AI holds the potential to fundamentally transform the approach healthcare payers adopt in managing and providing patient care. This cutting-edge technology has the capability to support payers in streamlining their operational processes, improving patient wellbeing, and mitigating financial burdens by creating new and unique data based primarily on existing datasets. According to an analysis done by McKinsey & Company, AI-enabled payer organizations can automate 50 to 75% of manual tasks, boosting efficiency to focus on complex cases and care delivery.
Several leading payer organizations have already started leveraging the benefits of GenAI. UnitedHealth introduced Agent Virtual Assistant (AVA) with GenAI capabilities, including a chatbot that collects patient data, thus creating a 360-view of the customer profile, enabling personalized healthcare programs, and enhancing customer satisfaction.
In this blog, we’ll dive deep into how GenAI can transform some of the core business functions within the payer ecosystem.
Claims Management
GenAI and automation can be of significant value to the claims management cycle. But many payers have only scratched the surface when it comes to integrating these new technologies within their revenue cycle operations. Numerous repetitive tasks within the claims cycle, which often demand significant time investment and are susceptible to human fallibility, could benefit from processes streamlined and automated through GenAI. Some of the use cases of GenAI in claims management include:
1. Decrease Denials with Automated Patient Access
Patient access is the starting point of the revenue cycle process. It allows patients to register, schedule appointments, collect insurance information and accumulate co-pays or deductibles. Interestingly, a substantial portion – ranging from 30% to 50% – originates from this juncture. Physical processes, unavailability of real-time insurance verification, and incorrect patient information contribute to the number of denials. More than 80% of patients say they prefer an online registration experience. GenAI-backed patient intake software can empower patients to conveniently complete registration forms at their convenience, fostering an improved experience while reducing denials and thus mitigating delays in reimbursement processes.
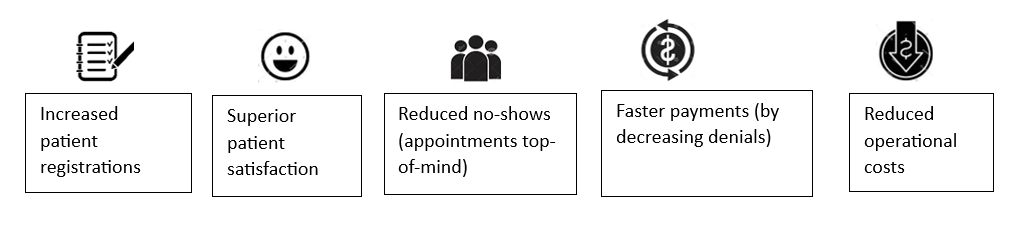
Benefits of GenAI-enabled Automated Patient Access
 2. Improved Patient Matching to Reduce Claims Denials
2. Improved Patient Matching to Reduce Claims Denials
One- The standard solution includes an enterprise master patient index (EMPI); however, EMPIs rely on a single data source-the patient rosters. If there are any inaccuracies in the patient roster, it can create issues in matching the patient records. Patient matching done via a GenAI-enabled platform simplifies patient identity management through a patient identifier assigned to each patient for authenticating and resolving any patient identity issues while safeguarding privacy concerns.
3. Efficient Claims Verification
The claims team usually does the guesswork on the probability of a denial, based on their experience and data, but turning those insights into an efficient process is difficult. ML tools backed with GenAI remove the guesswork by analyzing the denied claims, finding out the root cause, and using that data to predict future denials. Also, it can flag at-risk claims, prompting further comprehensive scrutiny through additional checks.
4. Reduced Denials with Automated Claims Management
Monitoring claim status in the adjudication process is essential for improving cash flow and maintaining a financially sound revenue cycle. GenAI-powered platform can eliminate manual follow-ups, enabling payers to respond early and accurately to pended, denied, or zero-pay transactions before the Electronic Remittance Advice and Explanation of Benefits are processed. Automated and timely status monitoring based on each payer’s adjudication timeframe improves productivity and facilitates accurate payment. It can also be leveraged to streamline triage by prioritizing claims and thus increasing revenue.
Back-office Operations Transformation Leveraging NLP with GenAI
Natural Language Processing (NLP) can help with information extraction, conversion of unstructured data to structured data, and document categorization. NLP with GenAI can help with efficient billing. It can extract relevant information from unstructured physician notes and appropriately assign medical codes to facilitate claims and, ultimately, the billing process. This is how it works:
1. Claims Data Extraction and Validation
NLP parses and extracts relevant information from medical claims to convert them into standardized codes. GenAI then facilitates the creation of organized claim data summaries, thereby enhancing precision and mitigating potential inaccuracies.
2. Billing Query Resolution
NLP interprets billing inquiries from providers, members, or staff. GenAI then generates detailed responses to billing queries, providing clear explanations and thus reducing response times.
3. Prior Authorization Optimization
NLP reviews clinical documentation to determine the medical necessity of treatments. GenAI then assists in generating prior authorization requests or recommendations based on NLP analysis by streamlining the process and reducing delays.
4. Fraud Detection and Billing Anomalies
NLP identifies irregular billing patterns or potentially fraudulent activities. Generative AI plays a pivotal role in generating notifications or comprehensive reports, identifying questionable billing practices, thereby fortifying the capabilities of fraud detection initiatives.
Customer Support
In contrast to chatbots and obsolete Interactive Voice Response (IVR) systems, GenAI conversational agents offer a distinct advantage by delivering personalized, human-like assistance with remarkable speed and scalability. These agents serve as a reliable source of up-to-date information on healthcare coverage, claims payment status, and related matters, thereby contributing to enhanced clarity and member satisfaction. GenAI in customer support can be leveraged as follows:
1. Member Services
- Create custom coverage summaries for specific benefits questions (online and via call-center contacts).
- Generate call scripts and other content for outbound nonclinical communications.
- Deploy adaptive chatbots and smart routing to assist in answering service questions for members and providers.
- Propose clinicians based on defined parameters, such as coverage, location, preferences, and conditions.
2. Provider Relationship Management
- Compare plan/product features and networks.
- Generate standard communications, such as welcome letters, reports, new member needs, claim denials, etc.
- Summarize gaps in provider directories, generate reports and observations, and review overall performance and identify loopholes for providers and vendors.
Personalized Healthcare Plans
Generative AI, along with advanced analytics, can generate healthcare recommendations. These plans can be tailored to individual preferences, thus improving customer experience while also reducing costs by leveraging real-time data and machine learning algorithms. This is how GenAI generates personalized healthcare plans:
1. Member Data Analysis and Assessment: GenAI analyzes comprehensive member data, including medical history, claims records, behavioral and mental health data (emotional patterns), and lifestyle information (diet, exercise, sleep, and stress levels). It identifies patterns, trends, and risk factors to gain insights into each member’s health profile while factoring in genetic predispositions, historical data, socio-demographic factors, and clinical indicators.
2. Personalized Recommendations: Generative AI algorithms process these individual patient/member data to create personalized health recommendations. These recommendations can include disease prevention strategies, medication regimes, dietary plans, exercise routines, and mental health support.
3. Telehealth and Remote Monitoring: GenAI can generate personalized telehealth plans, facilitating virtual consultations and remote health monitoring. It can provide guidance on using telehealth platforms and tracking health metrics.
4. Member Education and Engagement: GenAI can generate personalized health education materials, making it easier to understand medical concepts and therapeutic alternatives through user-centric language in mobile apps or web interfaces. This enhances patient satisfaction and engages members in proactive self-care.
Incorporating Generative AI into your business strategy holds the potential to facilitate the expansion of your organization, expedite operational processes, drive cost efficiencies, and seamlessly integrate novel business paradigms while maintaining a competitive advantage to stay ahead in the game.
How can Hexaware help you stay ahead?
By harnessing the power of GenAI, healthcare payers can navigate complexities with newfound agility, delivering unparalleled efficiency, accuracy, and value across every facet of their operations. Hexaware offers a blend of industry insights and technological proficiency at the convergence of responsible AI.
Our GenAI-powered Comprehensive Services
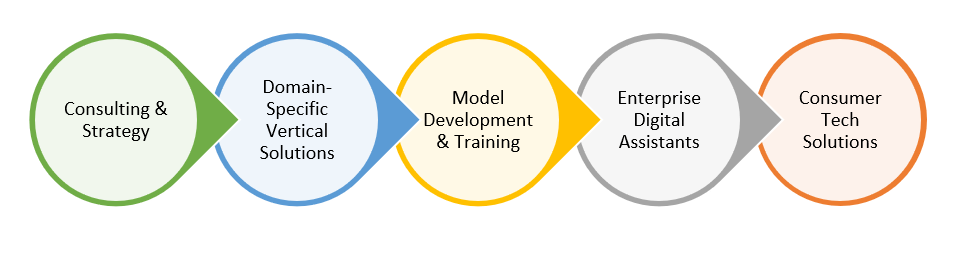
Hexaware presents a holistic solution tailored for healthcare payers venturing into their GenAI expedition. Contact marketing@hexaware.com to learn more.